1. Costs of care in patients with psoriatic arthritis and psoriasis
The costs of psoriasis and psoriatic arthritis (PsA) are substantial for both patients and the U.S. healthcare system. In this study, researchers compared healthcare resource use and costs in three groups: patients with psoriasis, patients with PsA, and matched controls without psoriasis or PsA in the United States.
To do so, they employed the IBM MarketScan commercial database with the goal of identifying three groups of adult patients, from January 1, 2009, through February 29, 2020, reviewing patients with psoriasis: ≥ 1 inpatient or 2 outpatient psoriasis diagnoses and no PsA diagnoses; patients with PsA: ≥ 1 inpatient or 2 outpatient PsA diagnoses; and control: no psoriasis and PsA diagnoses. Controls were matched 1: 1 with patients with psoriasis and PsA according to age, sex, and comorbidities. Healthcare resource utilization and costs (in 2019 USD) were assessed descriptively and by mixed models over 5 years of follow-up.
Reviewing the results, we find that 208,434 patients with psoriasis and 47,274 patients with PsA were matched with the control group (N = 255,708) and the annual all-cause health care costs per patient were $7,542, $11,856, and $29,621 for the control, psoriasis and PsA groups, respectively.
Meanwhile, all-cause health care costs were significantly higher among patients with PsA and patients with psoriasis than controls at 1 year. These costs were also significantly higher for patients with PsA than in patients with psoriasis at 1 year.
This trend of increased costs for patients with PAs compared to the rest of the groups was maintained throughout the five years of follow-up and in all categories of healthcare resources, the highest use was among patients with PAs and lower in the control group.
Categories included hospitalizations, physician office visits and outpatient hospital services, radiology, emergency room, laboratory, and outpatient pharmacy.
Finally, the researchers concluded that annual health care costs and resource utilization were significantly higher for patients with PsA compared to patients with psoriasis and the control group. The differences in cost and resource utilization between these patient groups highlight the higher disease burden for patients with PsA compared to patients with psoriasis or patients without either of these diseases.
- Reproductive health in women with rheumatic diseases
Autoimmune rheumatic diseases (ARDs) commonly affect women of childbearing age. In the case of active maternal disease in the months prior to conception increases the risk of flares during pregnancy, which increases the risk of adverse pregnancy outcomes. Therefore, maternal, and fetal health can be optimized by planning conception when the disease is controlled so that a treatment regimen can be maintained throughout pregnancy. This study aims to perform the construction and validation of a Reproductive Health Questionnaire (RHQ) for patients with ARD.
To analyze, a validation and construction of a RHQ in women of reproductive age with ARD was carried out in two phases.
In the first one, a review of the literature and the construction of the questionnaire was made by a multidisciplinary team of experts and, in the second one, a cross-sectional study was executed to complete the validation and estimate Cronbach's alpha based on the tetrachoric correlation coefficients, the correlation matrix and the Cohen's kappa test coefficient. Instrument stability was measured by comparing two measurements on the same study subject with a time lag between them.
Among the results, for example, in the first phase, a 38-question instrument was developed (some were modified due to confusion or discomfort caused to some patients) and more response options were added.
In the second phase, version 5 of the RHQ was applied to 100 women with ARD, with an average age of 35 years. The most frequent disease was rheumatoid arthritis (54%), finding a difference of 6 months between the onset of disease symptoms and diagnosis. The correlation matrixes showed good correlations in dimensions 3, 5, 6, 6, 7 and 9 (0.53, 0.82, 0.92 and 0.452 respectively), in addition, difficulties were identified in two dimensions, so they were restructured.
For the researchers, the main conclusion is based on the fact that the RHQ is a useful and practical tool to assess reproductive health (fertility, reproductive preferences, contraception, counseling, sexuality, and breastfeeding) in women with ARD and could help with timely intervention on reproductive health problems, decreasing adverse fetal and maternal outcomes.
- Covid patients with rheumatic diseases
The researchers performed a comparison of characteristics of patients with rheumatic disease and covid-19 in Argentina and contrasted them with data reported at the Latin American and global level (Global Registry International Alliance RheumCOVID).
For this purpose, a national, multicenter, prospective, and observational registry was conducted and patients over 18 years of age, with a diagnosis of rheumatic disease and SARS-CoV-2 infection by PCR or positive serology, were included between August 13, 2020, and April 11, 2021. Demographics, baseline rheumatic disease, comorbidities, clinical-laboratory characteristics of SARS-CoV-2 infection, as well as treatments and outcomes were used.
Statistical and descriptive comparisons were performed using ANOVA, chi2 or Fisher's test.
A total of 863 patients from Argentina, 74 from Latin America and 583 from the rest of the world were included, mostly women in the three groups (79.4%, 73% and 71% respectively).
The most frequent rheumatic diseases in the three groups were found to be rheumatoid arthritis (45.8%, 35% and 39%, respectively) and systemic lupus erythematosus (18%, 22% and 14%).
Another finding had to do with the fact that in Argentina fewer patients received specific pharmacological treatment for covid-19 than in the other 2 groups (41.4%, 68% and 43% respectively, and there was less need for non-invasive/invasive mechanical ventilation than in the rest of Latin America and the world (8.6% vs. 31% vs. 13%).
Likewise, the researchers point out, the need for hospitalization in Argentina was lower than in the rest of Latin America and the rest of the world (32.8% vs. 61% vs. 45%), as was mortality (5.8%, 12% and 11%).
On the other hand, they reported that 86.9 % of the patients did not present complications in Argentina, with a statistically significant difference with the rest of the groups (62 % and 77 %).
Among the conclusions, the group of researchers highlighted that patients with rheumatic diseases and SARS-CoV-2 infection from Argentina reported in this registry received less specific pharmacological treatment for covid-19 than those registered in other countries, presented fewer complications, and required less ventilatory support.
When reviewing the mortality data, although it was lower in the Argentine registry, the fact that the registries have information collected at different times of the pandemic and different local epidemiological situations does not allow conclusions to be drawn in this regard.
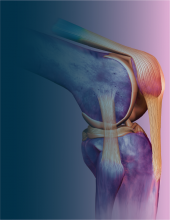
- Metabolic syndrome in patients with psoriatic arthritis.
With the aim of studying the prevalence of the metabolic syndrome in patients with psoriatic arthritis and the correlation between obesity and PsAID 12 score, the researchers conducted a multicenter cross-sectional study with a total of 160 patients who met the Classification of Psoriatic Arthritis (CASPAR) criteria, who were recruited from six Brazilian rheumatology centers.
The metabolic syndrome (MS) was defined according to the criteria of the Adult Treatment Panel III (ATP III) of the National Cholesterol Education Program (NCEP) and obesity according to Body Mass Index (BMI).
The association of BMI with PsAID-12 was evaluated using Spearman's correlation coefficient and the significance level adopted was 5%. About the method, the researcher highlights, it can be said that of the 160 patients included, 50 % were women, with a mean age of 54.0 ± 11.2 years. Regarding psoriatic disease, 68 % had only peripheral arthritis and 32 % had pure or mixed axial alteration. The prevalence of MS was 62.5 % and obesity was present in 34.4 % of all patients.
In this case, there was a statistically significant positive association between BMI and PsAID-12 total score: the higher the degree of obesity defined by BMI, the higher the PsAID-12 scores.
Among the results, they report that in the experience of the research group, MS was present in more than 60% of patients and the PsAID-12 score correlated with obesity: obese patients had a significantly higher impact of psoriatic arthritis as measured by the PsAID-12 score.
- Differential characteristics of patients with psoriatic arthritis
Reviewing that many authors have established the frequency of psoriatic arthritis (PsA) in patients with psoriasis (PsO) (33%), but not in clinical musculoskeletal pain (MSK), the objective of the researchers was set to estimate the frequency of PsA in a cohort of patients who consulted for polyarthralgia and to evaluate the differential characteristics of these patients in relation to patients with final diagnosis other than PsA.
Given this, a prospective cohort study was used, which included patients older than 18 years who were admitted for arthralgias to the Reumacheck program (2017-2020).
Laboratories, radiographs, hand ultrasound with power Doppler (22 joints) and interview (sociodemographic, clinical, clinimetry) were performed. Each evaluator did not know the data of the other studies.
At subsequent visits (patients who completed at least 2 visits were included), the results were evaluated and the definitive diagnosis of PsA was established according to CASPAR criteria. Chi2, Fisher's exact test, Student's t-test, MW, and multivariate logistic regression analysis were performed using PsA as the dependent variable.
The process included 746 patients with polyarthralgia (74.4 % women, mean age 53.6 years), of whom 71 (9.5 %, 95 % CI: 7.6-11.8) had a final diagnosis of PsA.
In addition, no significant differences were found regarding the presence of comorbidities such as diabetes mellitus, arterial hypertension, and dyslipidemia (17.6 % vs 12.3 %, p = 0.21, 34.3 % vs 31 %, p = 0.57 and 20.5 % vs 21.4 %, p = 0.86, respectively).
However, significant differences were found in smoking, 57.5% (PsA) vs. 42.4% of controls. In multivariate analysis, PsA was associated with PsO (OR: 563.3, 95 % CI: 53.2-5966), family history (OR: 102.9, 95 % CI: 11-958.2), number of swollen joints (OR: 1.4, 95 % CI: 1.02-2.19), radiographic erosions (OR: 9.5, 95 % CI: 1.1-80.8) and ultrasound with at least one joint with positive PD signal (OR: 20.2, 95 % CI: 2-203.2). On the other hand, it was negatively associated with positivity for rheumatoid factor (OR: 0.1, 95 % CI: 0-0.18).
The researchers conclude that the frequency of PsA in this cohort was 9.5%, it was associated with personal and/or family history of PsO, greater number of swollen joints, radiographic erosions, and the presence of hand ultrasound with Power Doppler signal at joint level. On the other hand, the presence of RF was shown to be a protective factor.